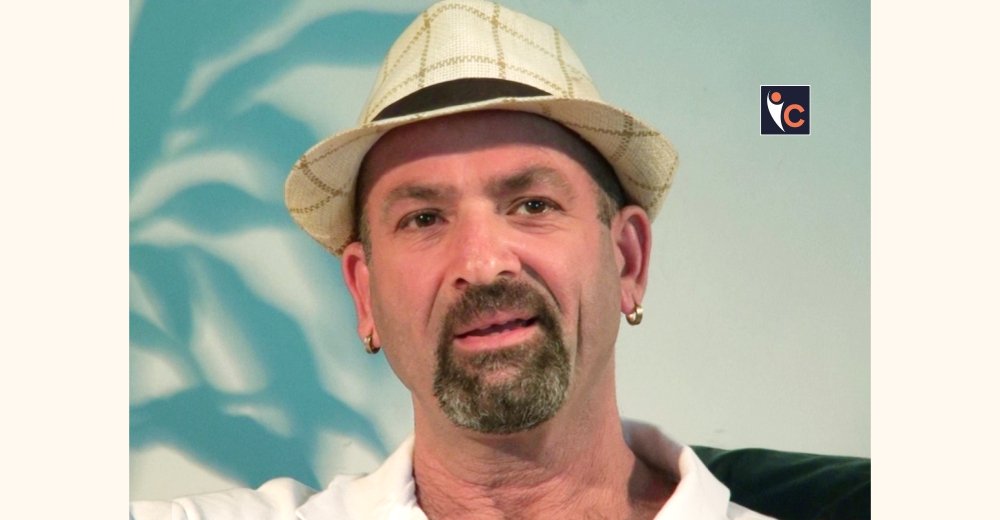
At the Interventional Pain Management, Spasticity & Neuromodulation Unit at Hygeia Hospital in Athens, Greece, Georgios Matis MD, MSc, PhD, FINR(CH) is presented as the clinician leading an approach that unites science, technology, and humanism. The unit’s philosophy views pain relief as the restoration of a person’s narrative rather than the simple reduction of symptoms.
Dr. Georgios Matis oversees a program that includes spinal cord stimulation using FAST, Contour, DTM, and BurstDR waveforms, multifidus stimulation, peripheral nerve stimulation, radiofrequency procedures, closed-loop spinal cord stimulation, remote programming technologies, and an intrathecal therapy program featuring ziconotide.
His perspective is also shaped by his roles as Editorial Board Member of Neuromodulation: Technology at the Neural Interface, Co-Chair of the INS Medical and Public Education and Engagement Committee, Secretary of the German Society for Neuromodulation, and active member of the Canadian Neuromodulation Society.
Let’s delve into the interview details below!
What inspired the creation of your unit, and how has its mission evolved over time?
The inspiration for this unit emerged from a conviction that pain medicine required a new architecture; one as bold and humanistic as the sculptures of Gian Lorenzo Bernini, whose works captured both the fragility and magnificence of the human condition. For years, patients had navigated fragmented systems of care, often feeling unheard. The creation of this unit sought to challenge that landscape by building a place where interventional pain therapies and neuromodulation could coexist with empathy, precision, and scientific rigor. Over time, the mission expanded beyond clinical care. As the field evolved with AI-enhanced neuromodulation, closed-loop spinal cord stimulation, and advanced waveforms that offer unprecedented personalization, our vision matured into something larger: an institute of continuous learning, research, and global exchange. This evolution mirrors the musical revolution of Johann Sebastian Bach, whose compositions grew not only in complexity but in societal influence. Today, the mission also reflects my journey as an author of several key works—Intrathecal Therapy and Ziconotide, From Surgeons to Storytellers, Pain and Pulses, Recent Developments in Spinal Cord Stimulation, and as editor of The Handbook of Neuromodulation. With the forthcoming release of Neuromodulation as Art, our unit embraces the belief that medicine must move beyond technique and into meaning: a philosophy that continues to shape our identity and aspirations.
Which key therapies, technologies, or methods distinguish your unit in 2025?
In 2025, our unit stands at the vanguard of neuromodulation, offering an array of therapies that reflect the bold experimentation of artists like Wassily Kandinsky, whose abstraction redefined perception. Our portfolio includes closed-loop SCS, AI-driven programming, FAST, Contour, DTM, and BurstDR waveforms, multifidus stimulation, peripheral nerve stimulation, and radiofrequency procedures, all integrated into a refined clinical ecosystem. Our intrathecal therapy program, anchored by therapies such as ziconotide, provides a lifeline for patients with refractory pain, while our adoption of remote programming and digital monitoring ensures continuity of care across international borders. This combination of precision and accessibility makes our unit one of the most technologically advanced in Southeastern Europe. What further distinguishes us is our commitment to intertwining science with the humanities. Our forthcoming academic contributions including, Neuromodulation as Art, serve as a testament to our belief that medicine must embrace creativity, narrative, and the spirit of exploration. This holistic fusion shapes both our clinical outcomes and our institutional identity.
What measurable patient outcomes or transformations best demonstrate the impact of your approach?
The transformations we witness are often as profound as the novels of Leo Tolstoy, rich in depth and marked by moments of human awakening. Patients who once lived in the shadows of chronic pain now walk freely, restore their family roles, and reconnect with activities long abandoned. These narrative shifts are supported by measurable reductions in pain scores, improved functional metrics, enhanced sleep quality, and demonstrable gains in mobility and emotional wellbeing. Our neuromodulation outcomes whether through closed-loop SCS, advanced waveforms, multifidus stimulation or peripheral nerve stimulation reflect consistent improvements in both short- and long-term follow-up. Remote monitoring ensures stability of therapeutic effects, allowing for rapid, data-driven adjustments that preserve patient progress. In intrathecal therapy, ziconotide continues to demonstrate valuable efficacy in cases previously considered untreatable. Each transformation, however, is more than a statistic. It is a testimony to the guiding principle that care must extend beyond the procedural and into the personal. When patients regain autonomy, purpose, and dignity, we see the true measure of our success.
How does your team collaborate across disciplines to deliver truly comprehensive care?
Our collaborative approach resembles the architectural harmony of Antoni Gaudí: diverse elements woven together into a structure that feels organic, unified, and purposeful. Physicians, nurses, physiotherapists, psychologists, and specialized neuromodulation programmers converge with a singular aim: to elevate patient outcomes. Interdisciplinary meetings allow for nuanced discussions on waveform programming, AI-driven analytics, optimal lead placement, intrathecal therapy choices, and long-term strategies for complex pain syndromes and spasticity. This synergy ensures that no detail is overlooked and no patient is treated with a one-size-fits-all approach. The insights shared between specialists foster a collective intelligence greater than the sum of its parts. Our global affiliations through the INS, German and Canadian Neuromodulation Societies, and international collaborations reinforce this teamwork with ongoing access to knowledge and evolving best practices. Together, we create an environment where innovation thrives and patient care reaches its highest potential.
What emerging trends or research developments in integrative health are shaping your unit’s future direction?
Our future direction is guided by emerging trends that echo the intellectual curiosity of Leonardo da Vinci: an insatiable desire to observe, understand, and transcend limitations. Among the most transformative developments are AI-enhanced neuromodulation, machine-learning-based waveform optimization, and the evolution of closed-loop systems that respond dynamically to physiological signals. We are also exploring advances in brain-spine interfacing, digital phenotyping, and expanded capabilities for remote programming, which allow patients (whether in Greece, Germany, Switzerland, or Cyprus) to receive real-time, expert-level adjustments from afar. Multifidus stimulation and innovations in peripheral stimulation continue to gain scientific traction, opening new pathways for rehabilitation and biomechanical restoration. These trends reinforce our commitment to remain trailblazers in neuromodulation research and clinical practice. They also align with our broader vision to integrate science and art within medicine, an approach that will be fully expressed in my upcoming book, Neuromodulation as Art.
What meaningful advice would you offer individuals beginning their journey with integrative health care?
To those embarking on this journey, I often recall the wisdom of the poet Sappho, who wrote that “whatever you love, you will pursue.” Healing begins with the courage to pursue your own wellbeing, to trust that transformation is possible and that suffering does not define your identity. Integrative health invites you to engage actively, to ask questions, and to participate fully in your care. Whether your treatment involves neuromodulation, pharmacotherapy, physical rehabilitation, or psychological resilience training, the process works best when you stand as a co-author of your healing story. Much like Igor Stravinsky reshaped musical form through bold experimentation, your journey may require openness to new methodologies, technologies, and ways of thinking. Finally, remember that treatment is a partnership. Our team will walk beside you with empathy and expertise, offering therapies that span from spinal cord and multifidus stimulation to intrathecal ziconotide therapy and AI-guided adaptations. Together, we aim not only to reduce pain but to restore meaning, function, and vitality to your life.
Integrative Care Model
Dr. Georgios Matis defines the unit’s integrative care model as the alignment of technological sophistication with humanistic care. The approach combines interventional techniques, neuromodulation therapies, advanced imaging, functional rehabilitation, and continuous follow-up supported by remote connectivity. Each patient is regarded as an individual with a unique story rather than a diagnosis.
The model’s effectiveness stems from personalized neuromodulation programming, remote technologies, and AI-assisted analysis to optimize stimulation parameters, waveform selections, dosing strategies, and adaptive closed-loop responses. Treatments include BurstDR, DTM, and multifidus stimulation, each tailored to patient needs.
The unit also provides cross-border care, supported by Dr. Matis’s licensure in Greece, Cyprus, Germany, and Switzerland, ensuring consistent access for patients across Europe.