Not so long ago, robotic surgery was considered a bold experiment, futuristic, intriguing, but far from routine. Fast forward twenty years, and at The University of Kansas Health System it is now part of everyday practice, trusted by patients and deeply integrated into surgical care. What started as a modest program has steadily grown into one of the region’s most comprehensive and forward-thinking initiatives.
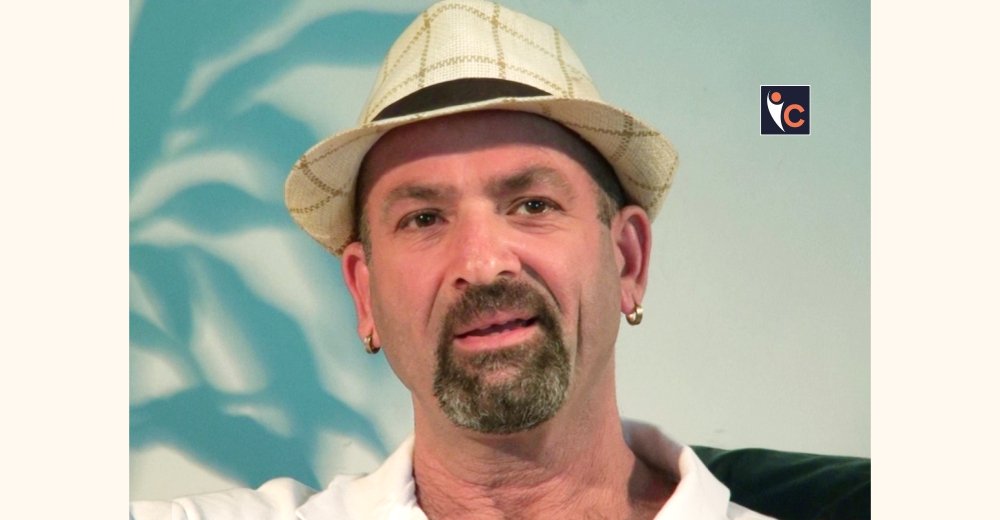
Driving much of this evolution is Dr. Moben Mirza, Urologic Oncologist and Chair of Urology at The University of Kansas Health System. Also a professor at the University of Kansas Medical Center, Dr. Mirza has helped bridge innovation in education and research with the realities of patient care. Under his leadership as director of the robotic surgery program, robotics has advanced from a promising technology to a defining part of the institution’s surgical identity.
It is not the machines that define the program, but the experts behind them: fellowship-trained surgeons, nurses, and staff who never stop learning. The newest generation of technology, such as the da Vinci 5 system, enhances this growth with iterative learning powered by machine learning and artificial intelligence. By providing real-time feedback on key performance metrics, it helps surgeons continuously refine their skills and ultimately improve patient outcomes.
More than anything, the program runs on teamwork and a commitment to do better every day. For patients, that leads to safer operations, quicker recovery, and real peace of mind.
Let’s delve into the interview details below!
Can you briefly introduce your robotic surgery center, including its history, core mission, and areas of specialization?
The University of Kansas Health System has been a pioneer in robotic surgery since 2005. A program that began with a single robot and two surgeons is now used across our health system’s surgical specialties and locations. The program began with the installation of the first soft tissue multiport robot, the DaVinci S System, on March 14, 2005. Initially, the program started with two robotic surgeons, but by 2025, it has grown to include 46. The program also now has 5 Xi robots, 1 SP robot, and 1 new DV5 robot. The program’s early focus was on urology procedures, but it quickly expanded to include gynecology, cardiac, thoracic, surgical oncology, ear nose and throat (ENT) and general surgery. Over the years, the health system has performed over 15,500 robotic surgeries, demonstrating its commitment to advancing minimally invasive surgical techniques.
Our core mission is to deliver the best patient care leveraging the technology at our disposal. Our surgeons are not just employing another tool, they are experts in their field and in robotic surgery. Our approach is programmatic and reflected in all the members of our well trained and experienced staff.
What inspired your center to invest in and advance robotic-assisted surgery, and how has that journey evolved over the years?
We saw robotic surgery as a natural evolution in our commitment to innovation and patient-centered care. Initially, it was about offering minimally invasive options for procedures. Over time, it has become a cornerstone of our surgical program – driven by evidence base approaches, strong outcomes, surgeon expertise, programmatic growth, and patient demand. What started as a desire for more minimally invasive options has grown into a multidisciplinary initiative with measurable impact.
What inspires us is our patient’s trust and our drive to achieve the best results for our patients.
What robotic platforms, tools, or technologies do you currently use, and how do they enhance surgical precision, patient safety, or recovery outcomes?
At our hospital in Kansas City, we currently have 5 Xi’s, 1 SP, and have now recently acquired a new DV5 robot (which is the next generation of the Xi). With the acquisition of this new system, we see all the benefits of the Xi but with added features such as ultra-high-definition 3D visualization, enhanced instrument precision, and next-generation haptic feedback that allows surgeons to feel weight and sense tissue resistance during procedures. These innovations help reduce trauma, improve accuracy, and support faster, safer recoveries.
How do you ensure your surgeons and medical teams are continuously trained and up to date on the latest robotic techniques?
We’ve built a standard of continuously learning. Our surgeons are experts who have specialized residency and fellowship training in their fields and application of robotic surgery. The surgeons participate in collaborative learning, simulation-based training, and peer to peer mentoring. We also host in house workshops for our residents and collaborate with Intuitive to stay ahead of the curve. Credentialing is rigorous, and we regularly review performance metrics to ensure safety and excellence. Our perioperative teams, operating room nurses, and surgical technicians have an intense training curriculum, extensive experience, regular refreshers, and are constantly cross-training. Our teams also travel for the most up-to-date hands-on skills and simulation training that they can bring back to the group.
Can you share any notable success stories or data points that reflect how robotic surgery has improved for your patients?
Notable success that we have made is expanding our single port robotic platform. We currently do SP cases in our ENT and urology service lines, but we are now starting to do cases in colorectal and thoracic. We are the only health system in the greater KC metro area that has a SP robot.
Is your center involved in any clinical research, trials, or partnerships related to robotic surgery advancements?
We have published data on many aspects of our fields of expertise that include robotic surgery. These data include improved patient outcomes, decreased length of hospital stay, improved quality of life outcomes, reduced blood loss and blood transfusions, faster time to recovery, and successfully pushing the envelope on more complex surgery. With the advent of the dv5, we hope to study the impact of haptic feedback for the surgeon and how it can translate and improve patient outcomes.
What trends or emerging technologies in robotic surgery are you most excited about for the future?
When we started our robotic surgery program, we would ask the question “which surgeries can we do robotically?” With increased experience and immense expertise, we now default to robotic surgery as the best option for our patients in the majority of our work. Technological advancement must be applied with our patients in mind and our prime motive to improve outcomes. Robotic technology has improved with the advent of haptic feedback bringing in a dimension which is uncharted. Single port robotic surgery is also picking up steam with new applications and evidence showing its advantages in certain surgeries. Remote surgery utilizing robotic technology is another advancement which is exciting. Other improvements like advanced displays, controls, and improved ergonomics are also very promising.
What advice would you offer healthcare leaders considering robotic surgery programs, and what should patients know when choosing a robotic surgery center?
Start with a clear vision and strong clinical champions. Robotic surgery isn’t just about the technology – it’s about building a team and a culture that embraces innovation. It is very important to have a strong partnership with the company that develops the technology. Intuitive Surgical has been a great partner for us in consistently helping us build and educate our teams, provide resources, and promote our culture.
For patients, it is important to know that you surgeon is an expert in their field, first and foremost. Many centers use robotic platforms for surgery. Our surgeons have obtained advanced training, fellowship specialization, and obtained a rigorous standard to practice in an environment of programmatic expertise. They can leverage the technology to deliver the best outcomes consistently. It is important for patients to ask about the surgeon experience, the experience of the institution, and the teams that support the surgeons. There is overwhelming evidence that patient outcomes are better in high volume and specialized center which is all available and more at The University of Kansas Health System.